
Chakan
Assisted Admission & Discharge Support
Insurance Claims Support
No-Cost EMI
4 days Hospitalization
| Knee Replacement Surgery Types | Estimated Recovery Days | Hospital Stay Duration | Age Group |
|---|---|---|---|
| Total Knee Replacement (TKR) | 4-8 weeks | 2-4 days | Typically 50+ |
| Partial Knee Replacement (PKR) | 2-6 weeks | 2-4 days | Typically 50+ |
| Minimally Invasive Knee Replacement | 3-6 weeks | 1-3 days | Typically 50+ |
| Revision Knee Replacement | 6-12 weeks | 3-5 days | Typically 60+ |
| Bilateral Knee Replacement | 8-12 weeks | 4-7 days | Typically 60+ |
| Custom Knee Replacement | 4-8 weeks | 2-4 days | Typically 50+ |
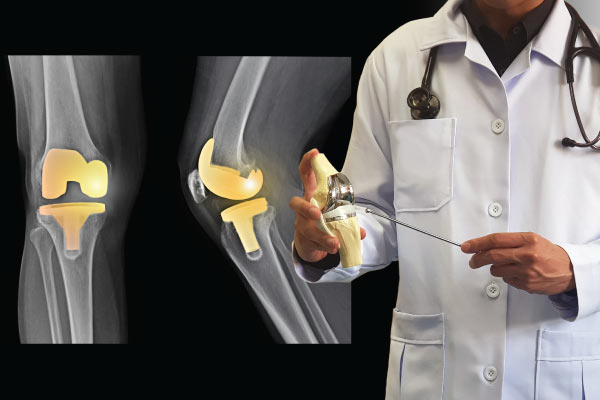
Knee replacement, also known as knee arthroplasty, is a surgical procedure to replace damaged or worn surfaces of the knee joint with artificial implants. It's typically recommended for individuals with severe knee pain and stiffness, often caused by conditions like osteoarthritis, rheumatoid arthritis, or injury. During the surgery, the damaged parts of the knee joint are removed and replaced with metal or plastic components to restore function and alleviate pain. Knee replacement surgery aims to improve mobility, relieve pain, and enhance the overall quality of life for patients.
The knee is a complex joint that connects the thigh bone (femur) to the shinbone (tibia). It consists of three main components - the femur's lower end, the tibia's upper end, and the kneecap (patella). Articular cartilage covers the ends of the femur, tibia, and back of the patella, allowing smooth movement within the joint. Ligaments, including the anterior and posterior cruciate ligaments and the medial and lateral collateral ligaments, provide stability to the knee. Additionally, the meniscus, two C-shaped pieces of cartilage, acts as a shock absorber between the femur and tibia, cushioning and stabilizing the joint during movement.
In India, knee replacement surgeries have seen a significant rise in recent years due to an aging population, increased prevalence of osteoarthritis, and improved access to healthcare services. According to data from the Indian Orthopaedic Association, over 200,000 knee replacement surgeries are performed annually in India, with numbers steadily increasing. This reflects the growing demand for joint replacement procedures to address the rising cases of musculoskeletal disorders in the country. With advancements in surgical techniques and implant technologies, knee replacement surgeries continue to offer promising outcomes for patients seeking relief from debilitating knee conditions.
Before undergoing knee replacement surgery, patients typically complete a thorough diagnostic process to assess the severity of their condition and confirm that surgery is the most appropriate course of action. Common evaluations include:

Knee replacement typically involves the following steps:
Best Healthcare Provider for Orthopedic Treatments
Minimally invasive knee replacement involves a much smaller incision of 4 to 6 inches, unlike traditional knee replacement, that involves a much longer incision of 8 to 10 inches.
Our Orthopedic Surgeons use the best prosthesis for joint replacement surgeries, such as Johnson & Johnson, Stryker, Zimmer, Smith & Nephew. Usage of the best quality implants for orthopedic procedures in order to promote longevity and durability.
The patient’s physiotherapy preferably begins after 10-12 days of surgery. For your smooth and precise recovery post knee replacement surgery, we will help you connect with the best Physiotherapist near you.
We offer follow-up consultations with the surgeon and provide instructions for post surgery care including dietary tips and exercises to our patients to ensure they have a smooth recovery.
There are typically 5 types of knee replacement surgeries:
Minimally-invasive Knee Replacement – This approach involves using smaller incisions and specialized surgical instruments to perform the procedure. This approach aims to minimize tissue damage, reduce blood loss, and accelerate recovery compared to traditional open surgery.
Before surgery, the patient undergoes a comprehensive medical evaluation, including a review of medical history, physical examination, and possibly additional tests such as blood tests, electrocardiogram (ECG), or imaging studies to assess overall health and identify any underlying medical conditions that may affect the surgery or recovery.
Patients receive detailed information about the knee replacement procedure, including what to expect before, during, and after surgery. This education may cover topics such as anesthesia options, surgical techniques, potential risks and complications, postoperative care instructions, and rehabilitation goals. Preoperative education helps patients feel informed and prepared for their upcoming surgery.
The healthcare team reviews the patient’s current medications and may make adjustments or provide specific instructions regarding which medications to continue or discontinue before surgery. This may include medications to manage chronic conditions, blood thinners, and supplements that could interfere with surgery or anesthesia.
Engaging in preoperative exercises and physical therapy can help strengthen the muscles around the knee joint, improve flexibility, and optimize overall physical fitness before surgery. This conditioning can enhance surgical outcomes, accelerate recovery, and facilitate postoperative rehabilitation.
Proper nutrition plays a crucial role in supporting healing and recovery after surgery. Patients may receive guidance on maintaining a balanced diet rich in nutrients, staying hydrated, and avoiding excessive alcohol and caffeine consumption in the days leading up to surgery.
Patients may need to make arrangements for assistance with daily activities, transportation to and from the hospital, and home modifications to facilitate mobility and accessibility during the recovery period. This may involve setting up assistive devices such as walkers or crutches, arranging for home care services, and ensuring a safe and comfortable recovery environment.
Knee replacement surgery is typically recommended for individuals with severe knee pain, stiffness, and functional limitations who have not responded adequately to conservative treatments such as medication, physical therapy, and lifestyle modifications. Some common indications for knee replacement surgery include:
Failed Conservative Treatments – When conservative treatments such as medication, physical therapy, corticosteroid injections, and joint supplements fail to provide sufficient relief from symptoms or improve knee function, surgery may be considered as a next step.
The decision to undergo knee replacement surgery is made on a case-by-case basis, taking into account factors such as the severity of symptoms, the impact on daily activities and quality of life, overall health, and individual treatment goals. Orthopedic surgeons carefully evaluate each patient’s condition and medical history to determine whether knee replacement surgery is the most appropriate treatment option to address their specific needs and improve their overall knee function and quality of life.
The recovery phase after knee replacement aims at restoring mobility, reducing pain, and regaining strength and function in the operated knee.
After surgery, patients typically spend a few days in the hospital for monitoring and initial postoperative care. During this time, pain management, wound care, and physical therapy begin.
Pain management strategies may include medications prescribed by the healthcare team, such as opioids for acute pain and nonsteroidal anti-inflammatory drugs (NSAIDs) for inflammation. As recovery progresses, pain management may transition to over-the-counter medications and other non-pharmacological interventions.
Physical therapy plays a crucial role in the recovery process, starting soon after surgery. Physical therapists work with patients to restore range of motion, strength, and flexibility in the operated knee through targeted exercises, stretching, and mobility drills. The frequency and intensity of physical therapy sessions may vary depending on individual progress and goals.
Patients are encouraged to begin walking and weight-bearing on the operated leg with the assistance of crutches, a walker, or other mobility aids as directed by the healthcare team. Gradually increasing activity levels and gradually weaning off assistive devices help promote healing and prevent complications.
After discharge from the hospital, patients continue their recovery at home with guidance from the healthcare team. This may involve following a prescribed exercise program, adhering to postoperative precautions (such as avoiding certain movements or positions), and attending outpatient physical therapy sessions as needed.
As recovery progresses and the knee strengthens, patients gradually resume activities of daily living and may eventually return to more demanding activities such as walking, climbing stairs, and recreational sports. The timeline for returning to specific activities varies depending on individual factors such as age, overall health, and the extent of preoperative impairment.
Generally, a knee implant is made of four components, i.e., a tibial component, a femoral component, a patellar component, and a plastic spacer. Based on their components, knee implants can be categorized as:
Knee replacement surgery usually takes between 3–4 hours. The time may vary depending on the type of knee replacement you have. For example, a total knee replacement can take 3 hours or more, while a partial knee replacement normally takes a little less than that.
A knee replacement can last 15–20 years for most people. However, the artificial knee parts may become loose or worn after 15–20 years, which may require another surgery on the same knee.
After knee replacement surgery, most people can walk independently with sticks after about a week, but this can vary depending on the individual. Patients are usually encouraged to start walking the same day with the help of a walker or other device.
Yes, physiotherapy is suggested after knee replacement surgery. Physical therapy helps improve the physical function of the knee and can help reduce risks after the surgery. Physiotherapy strengthens the muscles surrounding the operated joint and helps in recovery.
There is no ‘best’ age for knee replacement surgery. However medical practitioners consider that the optimal age for knee replacement surgery is between 70 to 80 years. According to medical reports available on the internet, most people who undergo knee replacement fall in the age group of 50 to 80 years.
While pain levels vary, knee replacement surgery typically involves significant discomfort during the initial recovery period, managed with medication and physical therapy. However, many patients report significant improvement in pain and mobility in the long term.
Yes, knee replacement is a major surgery. It involves anesthesia, incisions, and physiotherapy. The surgery is atypically a pretty complex one and demands stringent care while recovering.
Rehabilitation after knee replacement surgery involves a structured program of physical therapy and exercises aimed at restoring mobility, strength, and flexibility in the knee joint. This process typically begins shortly after surgery and continues for several weeks to months, focusing on reducing swelling, increasing range of motion, and regaining functional abilities for daily activities. Patient compliance and dedication to rehabilitation play crucial roles in achieving optimal outcomes.
For knee replacement surgery, you should consult an orthopedic surgeon in Chakan. They are medical specialists who are trained to perform knee replacement via different modern approaches.
.svg)
.svg)
.svg)